

Menopause is a natural phase in a woman's life, yet it can bring about significant changes and challenges. Fluctuating hormone levels, particularly estrogen and progesterone, can lead to a range of symptoms that affect physical and emotional well-being. Hot flashes, mood swings, and disrupted sleep are just a few examples of the many symptoms women may experience during menopause.
In such times, finding effective support is crucial to navigate this transitional phase with grace and comfort. This is where MenoRescue steps in, offering a solution designed to alleviate menopausal symptoms and promote overall health and balance.
MenoRescue is a specially formulated supplement crafted to provide targeted support during menopause. It combines carefully selected ingredients known for their beneficial effects on women's health, particularly during this phase of life. By addressing hormonal imbalances and supporting the body's natural processes, MenoRescue aims to help women manage menopausal symptoms and feel their best.
MenoRescue addresses menopausal symptoms from multiple angles, targeting both hormonal balance and overall well-being. By providing support for estrogen, progesterone, and cortisol levels, MenoRescue aims to mitigate common symptoms such as hot flashes, mood swings, and disrupted sleep patterns.

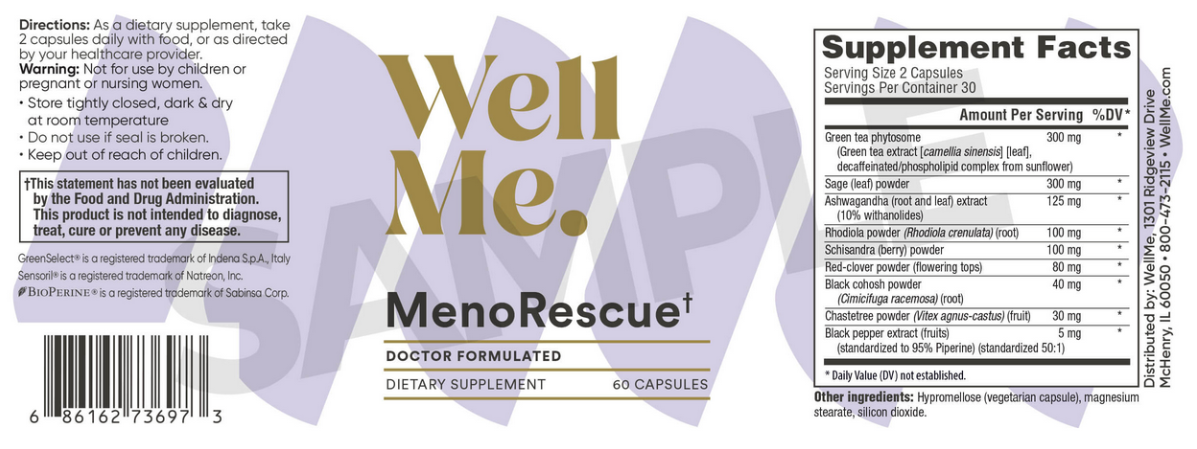
For optimal results, it is recommended to take MenoRescue supplement as directed by the manufacturer. Typically, this involves taking a specified dosage daily with meals. Consistency is key when using supplements, so it's important to incorporate MenoRescue into your daily routine for best results.
When starting MenoRescue supplement, it's essential to read the product label carefully and follow the recommended dosage instructions. This ensures that you're taking the correct amount for your individual needs and maximizing the benefits of the supplement.
It's also important to note any specific instructions regarding timing and potential interactions with other medications or supplements you may be taking. If you have any questions or concerns about taking MenoRescue supplement, don't hesitate to consult with a healthcare professional for personalized guidance.
In addition to taking MenoRescue supplement regularly, incorporating other healthy habits into your lifestyle can further enhance its effectiveness. Eating a balanced diet, staying hydrated, getting regular exercise, and managing stress levels can all contribute to overall well-being during menopause.
Consistency and patience are key when it comes to seeing results with MenoRescue. While some women may experience improvements in their symptoms relatively quickly, others may require more time to notice significant changes. It's important to give the supplement time to work and to stay committed to your health journey.

One of the primary challenges women face during menopause is maintaining hormonal balance. Estrogen and progesterone levels naturally decline during this phase, leading to a variety of symptoms. MenoRescue contains ingredients that support healthy estrogen and progesterone levels, helping to alleviate these symptoms and promote overall well-being.
In addition to hormonal changes, menopause can also be a stressful time for many women. Stress can impact cortisol levels, leading to further imbalance and exacerbating menopausal symptoms. The inclusion of rhodiola rosea in MenoRescue helps manage cortisol levels, allowing women to better cope with the stressors of daily life during menopause.
Unlike pharmaceutical interventions, which may come with unwanted side effects, MenoRescue offers a natural approach to menopause support. By harnessing the power of plant-based ingredients such as green tea and red clover, MenoRescue provides women with a safe and effective option for symptom relief.
Beyond symptom relief, MenoRescue also promotes long-term health and well-being during menopause. By addressing hormonal imbalances and supporting the body's natural processes, MenoRescue helps women feel their best as they navigate this transitional phase of life.
Navigating menopause can be challenging, but with the right support, women can experience this phase of life with greater comfort and vitality. MenoRescue offers a comprehensive solution designed to address menopausal symptoms and promote overall health and well-being. By harnessing the power of natural ingredients such as green tea, rhodiola rosea, and red clover, MenoRescue provides women with the support they need to thrive during this transitional period. With its money-back guarantee and commitment to quality, MenoRescue stands as a trusted ally for women seeking relief and balance during menopause.
